The digital transformation of healthcare has brought incredible innovations, from telemedicine to wearable fitness trackers. Among the most revolutionary advances is the integration of the Internet of Things (IoT) into medical devices. Connected medical technologies—such as pacemakers, insulin pumps, remote monitoring sensors, and even hospital equipment—are now part of a vast healthcare IoT ecosystem.
These devices improve patient outcomes by enabling real-time monitoring, data-driven treatment, and remote healthcare delivery. A patient with a heart condition can rely on a pacemaker that sends continuous data to a cardiologist. A person with diabetes can use a connected insulin pump to regulate glucose levels automatically. Hospitals can track ventilators and infusion pumps through centralized dashboards.
But the rapid adoption of IoT medical devices also introduces a new set of risks and vulnerabilities. Unlike traditional IT systems, medical IoT devices interact directly with the human body, meaning that failures or attacks can have life-or-death consequences. The combination of cybersecurity weaknesses, safety concerns, and regulatory challenges makes IoT in healthcare a double-edged sword.
This article examines the risks of IoT medical devices in depth, from cybersecurity and privacy to patient safety and interoperability. It also explores real-world incidents, regulatory frameworks, and the future of securing connected healthcare.
The rise of IoT in healthcare
IoT medical devices have seen explosive growth over the past decade. Market research shows that the global healthcare IoT market surpassed $250 billion in 2023 and is projected to reach nearly $500 billion by 2030. This expansion is driven by:
-
Chronic disease management: Devices like insulin pumps, glucose monitors, and pacemakers reduce hospital visits.
-
Aging population: Wearable sensors help monitor elderly patients remotely.
-
Hospital efficiency: IoT systems track equipment, beds, and supply chains in real time.
-
Preventive care: Continuous health data enables earlier detection of conditions.
Examples of IoT medical devices include:
-
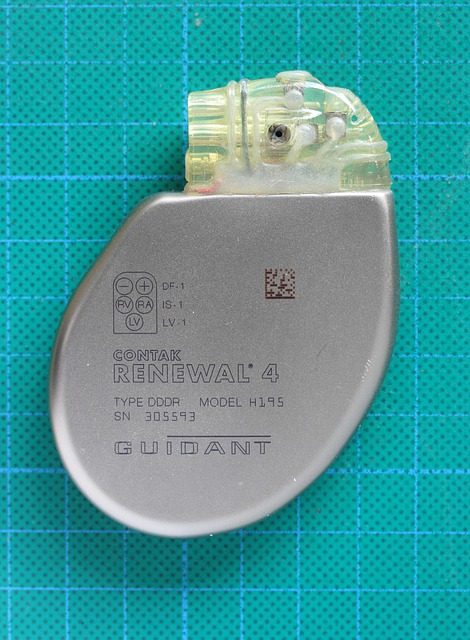
Implantable devices: pacemakers, defibrillators, neurostimulators.
-
Wearables: fitness trackers, ECG patches, smartwatches with medical sensors.
-
Infusion and insulin pumps: automated delivery of medication.
-
Remote patient monitoring systems: connected blood pressure monitors, oximeters.
-
Hospital devices: smart ventilators, connected imaging systems.
While the benefits are immense, the risks are equally significant. Unlike consumer IoT (like smart speakers), medical devices directly impact human health and safety.
Cybersecurity risks
Perhaps the most widely discussed risk is cybersecurity. IoT medical devices are prime targets for hackers because they often:
-
Run on outdated operating systems.
-
Lack proper encryption.
-
Use insecure wireless communication (Bluetooth, Wi-Fi).
-
Operate without regular patch updates.
Potential attack scenarios
-
Remote hacking of pacemakers
Security researchers have demonstrated the ability to remotely change the settings of pacemakers, potentially leading to dangerous heart rhythms. -
Manipulation of insulin pumps
Hackers could alter dosage settings, delivering too much or too little insulin, which could be fatal. -
Hospital ransomware attacks
Connected medical equipment can be taken offline as part of larger ransomware campaigns, disrupting patient care. -
Man-in-the-middle attacks
Intercepting data transmissions between devices and hospital servers to alter or steal medical data.
Cybersecurity for medical IoT is not just about protecting data—it’s about protecting lives.
Privacy and data risks
Medical devices generate enormous amounts of sensitive data: heart rates, insulin levels, brain activity, and more. This data, transmitted over networks and stored in cloud systems, is vulnerable to:
-
Data breaches: Hackers stealing health records to sell on black markets.
-
Unauthorized surveillance: Insurance companies or employers misusing medical data.
-
Identity theft: Health data used to commit fraud.
In the U.S., healthcare data is governed by HIPAA, and in Europe by GDPR. However, IoT devices often transmit data across borders and between third-party vendors, creating regulatory gray zones. Patients may not even know where their data is stored or how it is used.
Reliability and safety risks
IoT medical devices must function reliably in all circumstances. Failures can cause direct harm to patients. Key risks include:
-
Device malfunction: Software bugs or hardware failures in a pacemaker or pump can lead to medical emergencies.
-
Connectivity loss: A remote monitor losing connection may delay detection of a life-threatening condition.
-
Battery depletion: Many implantable devices rely on batteries with limited lifespans. Sudden power failure can be catastrophic.
-
Latency: Delayed data transmission may prevent timely interventions.
Unlike consumer IoT devices, medical IoT failures cannot be tolerated—reliability is paramount.
Interoperability challenges
The healthcare IoT landscape is fragmented. Devices from different manufacturers often:
-
Use incompatible communication protocols.
-
Fail to integrate with hospital information systems (EHR/EMR).
-
Lack standardized security frameworks.
This lack of interoperability increases risks:
-
Patients may need multiple apps for different devices.
-
Hospitals may miss critical alerts because of data silos.
-
Security is harder to manage when each vendor has different standards.
The absence of universal standards creates a patchwork system vulnerable to inefficiencies and errors.
Real-world cases of vulnerabilities
Several high-profile cases highlight the risks:
-
St. Jude Medical pacemakers (2017): The FDA confirmed vulnerabilities in pacemakers that could allow hackers to alter settings, leading to shocks or battery depletion.
-
Insulin pump recalls: In 2019, Medtronic recalled thousands of insulin pumps due to cybersecurity flaws that could let hackers control insulin delivery.
-
Hospital ransomware outbreaks: Attacks in Germany, Ireland, and the U.S. have forced hospitals to shut down connected equipment, delaying critical care.
These incidents demonstrate that IoT medical device risks are not theoretical—they are happening today.
Mitigation strategies
Stronger cybersecurity
-
End-to-end encryption of device communications.
-
Regular patching and software updates.
-
Secure authentication for device access.
AI-driven anomaly detection
Artificial intelligence can monitor device behavior and detect anomalies in real time, flagging possible tampering or malfunction.
Device certification and testing
Regulators and manufacturers must enforce rigorous security testing before devices reach patients.
Network segmentation
Hospitals can isolate medical IoT devices on separate networks to reduce attack surfaces.
User awareness
Patients and healthcare providers must be educated on safe device use and the importance of updates.
Regulatory landscape
Global regulators are beginning to address IoT medical device risks:
-
FDA (U.S.): Issues premarket and postmarket guidance for cybersecurity in medical devices.
-
European MDR (Medical Device Regulation): Requires risk management and security assessments.
-
HIPAA and GDPR: Impose strict data privacy requirements.
-
ISO/IEC standards: Efforts are underway to create security frameworks for connected health.
While progress is being made, regulations often lag behind the speed of technological innovation.
Future of IoT medical device safety
Looking ahead, several trends will shape the future:
-
Secure by design
Manufacturers will need to integrate cybersecurity from the ground up, not as an afterthought. -
Blockchain for medical data
Distributed ledgers may provide secure, tamper-proof storage of health records. -
Federated learning for privacy
AI models can be trained on decentralized health data without exposing patient information. -
Stricter liability frameworks
Laws may hold manufacturers accountable for device security failures. -
Global collaboration
Cross-border standards will be essential for securing IoT devices worldwide.
IoT medical devices offer enormous benefits for patients and healthcare systems. Pacemakers that communicate wirelessly, insulin pumps that adjust dosages automatically, and remote monitors that track vital signs have the potential to save countless lives.
Yet these same devices introduce unprecedented risks. Cybersecurity flaws, data privacy issues, reliability concerns, and lack of interoperability all threaten patient safety. Unlike other IoT systems, failure is not just inconvenient—it can be fatal.
The way forward is clear: IoT medical devices must be secure, reliable, and standardized. Manufacturers, regulators, healthcare providers, and patients must work together to ensure that innovation does not outpace safety. In the digital age of medicine, protecting devices means protecting lives.
Image(s) used in this article are either AI-generated or sourced from royalty-free platforms like Pixabay or Pexels.
Did you enjoy this article? Buy me a coffee!